There are medications for pain, but clinicians still struggle to heal patient suffering.
Suffering has to do with a threat to the patient’s identity – how they see themselves, how their family and friends see them and what they care about. Carol Taylor, a professor of medicine and nursing and a clinical senior scholar at Georgetown University’s Kennedy Institute of Ethics, explained how medical treatments only address part of a patient’s sickness. Just as important, she told National Press Foundation fellows: Spiritual care. That’s especially true for patients facing probable death.
In a study comparing end-of-life care, one in two patients reported that they did not receive enough emotional support. One in four expressed concern over physician communication and treatment options, and one in five said that dying patients were not always treated with respect.
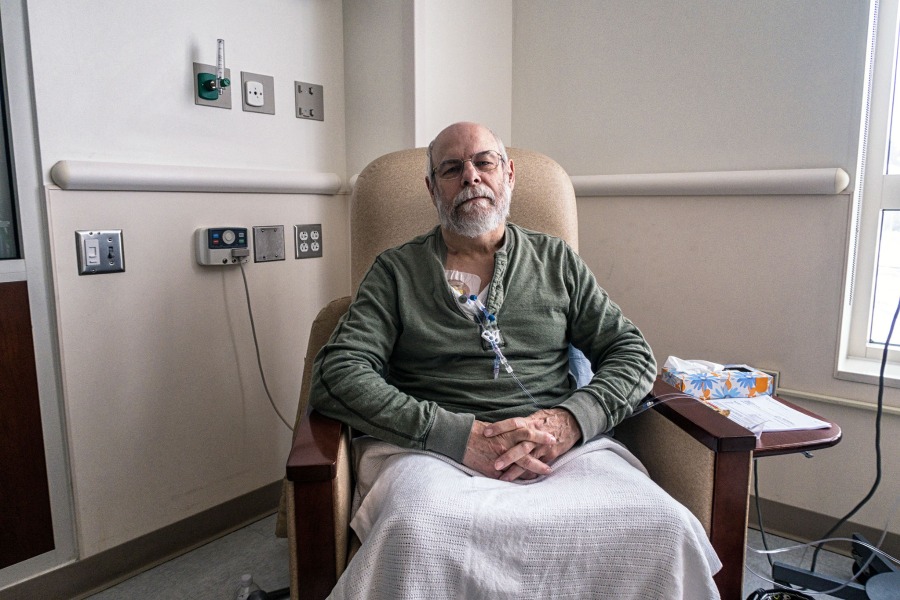
For Taylor, it’s personal. When Taylor’s brother was 35 years old, he was diagnosed with pancreatic cancer that couldn’t be treated with surgery. At the time, he was a recovering alcoholic with fractured family relationships. Taylor said that throughout treatment, her brother needed something to live for – or some glimpse of hope. Even as a practicing nurse, Taylor said her bag of tricks was frighteningly empty.
“We haven’t begun to address human suffering,” Taylor said.
Spiritual care goes beyond religion to include three components: The need for meaning and purpose, the need for love and relatedness, and the need for forgiveness. Patients who have been sick for years or are staring death in the face need these to come to terms with their diagnoses. That’s where palliative care comes in.

Taylor said the difference between palliative and hospice care is that hospice is meant to comfort and care for people who are likely to die within six months, while palliative care is about managing and alleviating spiritual and physical symptoms; it can start at any point in treatment.
In the past, Taylor said, palliative care started later in the treatment cycle as doctors focused on disease-modifying therapy early on. Now, however, oncologists see the importance of starting such palliative therapy at the point of diagnosis. Doing so can help with treatment decisions, feelings of helplessness and loneliness.
Palliative care methods are often overlooked as a moderate treatment for patients near death. Americans have struggled with the ethical and legal stipulations around a patient’s right to die, which is something many cancer patients may consider. Taylor said the two extremes for a patient facing death are to die a possibly painful death or to choose the time and manner of death. Strikingly absent: good palliative care as a medium option.
Taylor said physicians can mix spiritual care into their practices by focusing on healing as well as curing, which aims to make a patient feel whole and not scared of death. This, Taylor said, will ease a patient’s suffering.
“I don’t want to belong to a health care world where being a healing presence isn’t a part of who we are,” Taylor said.
This program is funded by the American Association for Cancer Research. NPF is solely responsible for the content.